| Download PDF (Available Soon) | |
| Author and Article Information |
Abstract
Background: Bystander cardiopulmonary resuscitation (CPR) has been shown to significantly improve survival from out-of-hospital cardiac arrest (OHCA), yet rates of bystander CPR remain low across the United States. Recent educational guidelines have identified hands-only CPR (HOCPR) training as an effective way to increase administration of bystander CPR and survival of cardiac arrest victims. Objectives: This study evaluates participants’ self-efficacy towards performing CPR before and after a brief, 5-minute HOCPR training to a collegiate population. Methods: An urban collegiate-based EMS agency conducted a one-day campus-wide HOCPR training event. Self-efficacy performing CPR before and after the brief training was measured on a reported comfort scale from 0 being “very uncomfortable” to 5 being “very comfortable.” Results: 410 participants were included in the study, with the proportion of participants reporting a self-efficacy level of 2 or lower decreasing from 69% before the training to 10% after the training. Conclusion: This paper outlines a brief HOCPR training that was successfully implemented by a collegiate-based EMS agency. Participants showed increased self-efficacy for CPR after the training, with potential implications of increasing administration of bystander CPR.
Introduction
More than 350,000 out-of-hospital cardiac arrests (OHCA) occur annually in the United States, posing a significant public health problem.1 Although less common, OHCA does occur on college campuses, affecting both students and members of the broader campus community.2 Overall survival from OHCA is under 10%, but prompt delivery of bystander cardiopulmonary resuscitation (CPR) can more than double survival for cardiac arrest victims.3-4 However, in the last 15 years, the prevalence of bystander CPR delivery was less than 40%, potentially contributing to low survival rates.1
Bystander CPR education is critical for increasing the rates of CPR administration and the subsequent survival of OHCA victims.5 In recent years, community education efforts have focused on Hands-Only CPR (HOCPR) training, which can be delivered to participants in under 5 minutes and at minimal cost.6 Consistent with research that emphasizes the importance of compressions when treating cardiac arrest,7 HOCPR for bystanders includes continuous chest compressions without rescue breaths.8 Previous studies have demonstrated the effectiveness of ultra-brief (<60 seconds) and brief (5 minutes) bystander HOCPR education programs on willingness to perform CPR and compression quality.9-11 Furthermore, participants expressed increased comfort performing CPR following a brief HOCPR training. Comfort and willingness to act are both components of self-efficacy, or a person’s perceived ability to perform a task correctly.12 OHCA victims living in communities with increased self-efficacy for CPR are more likely to receive bystander CPR,13 indicating the importance of widespread training.
Collegiate-based EMS organizations provide pre-hospital care on college campuses and are often student-led, allowing them to serve the unique needs of the campus community.14 One of the roles of collegiate-based EMS organizations is community education; promoting safety on college and university campuses by preparing community members to respond to emergencies. An urban collegiate-based EMS organization conducted a single-day, four-hour long campus-wide HOCPR training event. The purpose of this study is to evaluate the impact a brief, 5-minute HOCPR training had on participants’ self-efficacy for HOCPR as measured by self-reported comfort levels performing HOCPR. We also demonstrate the feasibility and impact of a campus-wide HOCPR education event conducted by a collegiate-based EMS agency. To date, there have been few investigations to evaluate the implementation of a brief, HOCPR training in a collegiate population.
Methods
Recruiting
The training event was conducted in February 2023 at a large private university (28,000 total students) in communal areas of dormitories, such as the main lobby and common lounges. Each station was equipped with a table featuring two CPR manikins, two emergency medical technicians (EMTs) to staff each station, and a laptop with a QR code leading to an electronic form was used for data collection. To incentivize participation, a variety of prizes were displayed, including merchandise from the university’s student health department, inflatable CPR manikins, CPR masks, organization-branded hot/cold packs, gift cards, and snacks. Upon completion of the CPR training and survey, participants were given the opportunity to spin a digital “prize wheel” to win one of the aforementioned prizes. No participants were excluded from the study.
Sample
The study utilized a convenience sample of the university community members who were willing to take part in the HOCPR training. Prior to the event, the training was advertised through social media and campus-wide email listservs. Participants (N=410) came from a passersby in dormitories and a dining hall. All 13 locations included in the study were on campus. Included in the study were university undergraduates (N=383), graduate students (N=12), faculty/staff (N=7), and non-university affiliates (N=8) (Table 1).
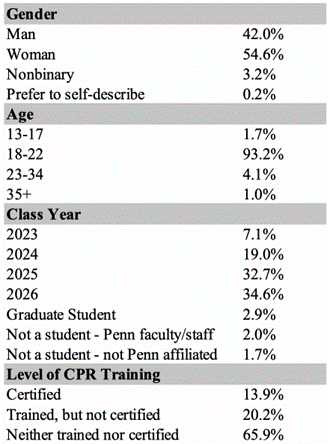
Table 1: Demographic information of study participants (N=410)
Data Collection
Data points were collected through a web-based survey (Qualtrics, Provo, Utah) that participants completed during the training. This study was considered exempt under university IRB regulations. The survey collected demographic information including age, gender, class year, and training location. No identifying information was collected from any individual.
Through the survey, we also looked to gauge participant experience and self-efficacy with CPR before and after training. We asked participants to fill out demographic information, history of CPR training or certification, when their most recent CPR training/certification was, and level of self-efficacy performing CPR prior to training. Self-efficacy was measured using a Likert scale, with 0 being “very uncomfortable” and 5 being “very comfortable.” This portion was done before the HOCPR training began. Immediately after training, participants were given the same Likert scale, and they evaluated their self-efficacy following the training.
Training Design
The trainings were conducted by 67 HOCPR instructors, all of whom were either campus EMTs or CPR-certified individuals who received additional training for this event, including preparation for student questions and discussion. During the trainings, participants were first introduced to the concept of HOCPR. Next, participants were taught to check for responsiveness in an unconscious individual. They were instructed to call 911 if they suspect cardiac arrest. Chest compressions were then demonstrated on CPR manikins by our HOCPR trainers. Trainees were advised to compress hard and fast and to the tempo of “Staying Alive” to maintain a compression rate of 100-120 compressions per minute. Participants demonstrated compressions for 60 seconds with trainers providing live feedback to ensure proper form and correct performance.
Data Analysis
We used non-parametric statistical tests to evaluate Likert scale data.15 We first verified that the median response of the pre-training data was 2 and the median response of the post-training data was 4. We also took 10000 bootstrapped samples of the pre- and post-training survey data to simulate a larger sample size and found that the median of the pre-training sample was 3 lower than the median of the post-training sample. To confirm a statistically significant difference, we conducted a paired t-test of the data and found a mean difference of 1.99 before and after training (p < 0.001). Given the discrete, ordinal nature of the Likert scale data, we also conducted a Wilcoxon signed rank test with continuity correction and found a significant difference in the location of the data before and after training with a median shift of 2.50 Likert points (p < 0.001).16
Results
The results of the statistical analyses demonstrate a significant change in reported self-efficacy performing CPR, indicating that the 5-minute HOCPR model may be effective in teaching the fundamentals of CPR. Furthermore, the difference in medians after bootstrapping suggests that replicating this training schematic on a larger scale may retain its effectiveness.
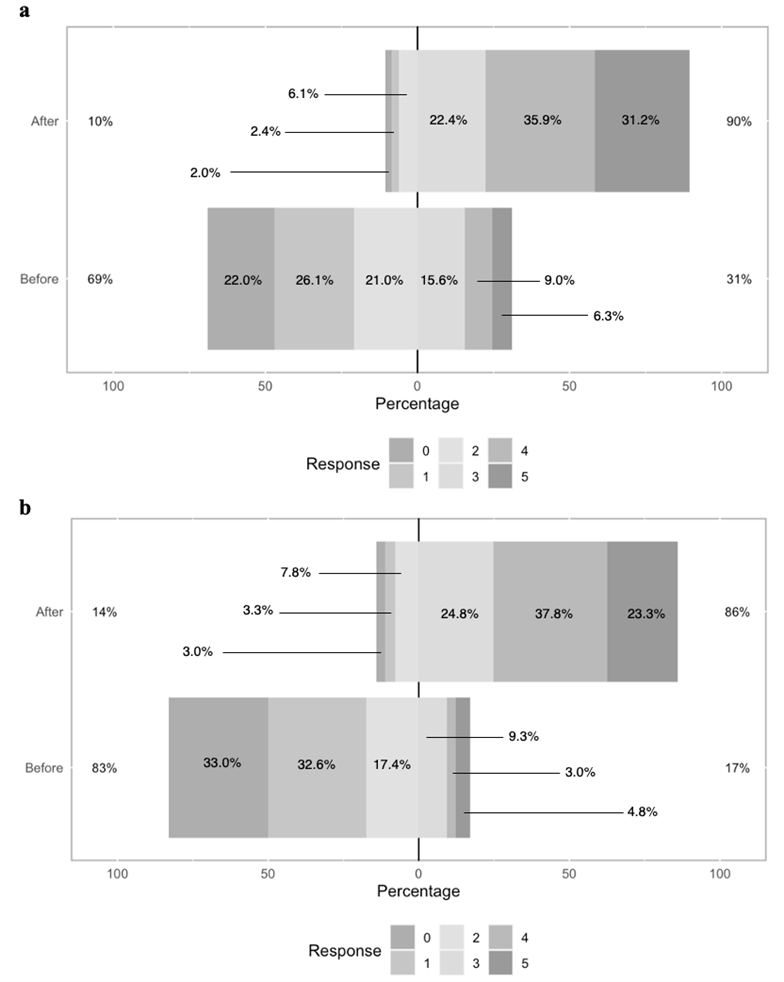
Before training, 69% of all participants answered 2 or lower on self-efficacy performing CPR and only a small proportion answered that they were very confident (Figure 1a). After the training, the number of respondents identifying with a score of 2 or lower dropped dramatically to 10%, with the proportion of people saying that they were not at all confident even smaller. A large proportion of respondents now had comfortability levels of 3, 4, or 5 (90%). The change in reported self-efficacy was even greater for individuals who had neither been trained nor certified in CPR, decreasing from 83% identifying with a score of 2 or lower before training to 14% after training (Figure 1b).
Figure 1: Change in reported comfortability levels before and after 5-minute HOCPR training for (a) all participants and (b) participants with neither CPR training nor certification.
Discussion
In this study, we demonstrate the impact of a brief HOCPR training in a collegiate setting, reporting a significant increase in reported self-efficacy from a majority of participants. The significance is based on existing literature supporting the importance of early/bystander CPR in OHCA. Bystander activation of emergency medical services (EMS) and rapid delivery of bystander CPR/defibrillation are key components of the American Heart Association (AHA) Chain of Survival,17 yet CPR is provided in less than 40% of cases.1 HOCPR community education has been proposed as a method of increasing rates of administration of CPR, as it reduces potential barriers like panic and hesitancy to perform mouth-to-mouth ventilation.18-19 In adults and teens who have witnessed OHCA, HOCPR is as effective, if not more effective, than conventional CPR due to simplified guidelines, bystanders’ increased willingness to perform CPR, and reduced interruption of compressions.20-22 Previous research has measured the impact of brief and ultrabrief HOCPR trainings on willingness to perform CPR and compression quality,9-11 but no studies have been implemented in a collegiate population. This study demonstrates the feasibility and impact of a campus-wide HOCPR training program conducted by a collegiate-based EMS agency.
The high community engagement, as well as the low cost barrier and low time commitment, of this HOCPR training model makes this an accessible outreach program for most collegiate settings. We recommend that other collegiate-based EMS agencies implement community HOCPR trainings to increase broader community knowledge in CPR. Although CPR education is mandated in 40 states within the U.S. as a high school graduation requirement,23 the actual number of students entering college with CPR training is lower. In 2017, the American College of Cardiology found that only 77% of the schools in states where CPR education is required indicated that they provided CPR education.24 Furthermore, although the exact time frame is unclear, CPR knowledge declines after initial training if not used or refreshed, indicating the need for continuous education following certification.25-26 Therefore, widespread CPR education on college campuses is an important and relevant community education program for collegiate-based EMS organizations to pursue.
Given that CPR knowledge requires continuous education to prevent decline, future research should assess follow-up training at different time points after initial training. By assessing how well CPR knowledge is retained after varying lengths of time, we can better understand the time frame of decline. Additionally, further studies could be optimized by implementing real-time feedback manikins to better assess the quality of CPR being performed.
Limitations
As this study was conducted on a university campus and primarily included students, this study is limited by the difficulty in interpreting the findings as representative of the broader U.S. population due to factors such as age and educational attainment. Furthermore, an unknown number of CPR-certified students declined participation in the study, which could have resulted in a biased sample. As a result, the study’s findings may not be generalizable to the broader campus population. Another limitation is the demographic makeup of the trainee population, as a majority consist of freshmen and sophomores, who are required to live on campus. In contrast, over 70% of upperclassmen at the university where the training was conducted live off-campus and make up only 26.1% of the participants. This could potentially limit the study’s external validity, as the findings may not apply to older or off-campus students who may interact less with on-campus resources. Follow-up analyses to evaluate the effectiveness of HOCPR training are challenging due to the anonymous nature of the survey, which makes it difficult to track participants and assess their performance during a real-life cardiac arrest event. Additionally, it is unclear whether the effects of HOCPR leading to increased self-efficacy immediately after training persist over time or decline at a predictable rate.
Conclusion
A brief HOCPR training was found to increase self-efficacy for performing CPR, increasing individuals’ self-efficacy performing HOCPR. This study also demonstrates the feasibility of a campus-wide HOCPR training conducted by a collegiate-based EMS agency. Accordingly, we encourage other agencies to pursue similar trainings. As the study was unable to assess the long-term impacts of a brief HOCPR training, future research should include randomized follow-up on training participants and use of real-time feedback manikins to assess CPR quality.
Acknowledgements
The authors would like to acknowledge Patrick Zhang for conducting the statistical analyses and creating the figures in RStudio. The authors would also like to acknowledge the Penn Center for Resuscitation Science, JHealth, Undergraduate Assembly, and Medical Emergency Response Team for their efforts during the training event. Lastly, they would like to thank Wellness at Penn, College Houses and Academic Services, and the Division of Public Safety for their support in planning the event.
The authors declare no conflicts of interest. The authors received funding from the Undergraduate Assembly and Center for Resuscitation Science to support the HOCPR training event.
References
1. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145(8). doi:10.1161/CIR.0000000000001052
2. Friedman NMG, Koenig GJ, Marks JA, Hilton MT, Glick JE. Characteristics and outcomes of cardiac arrests reported in the National Collegiate Emergency Medical Services Foundation data registry. Journal of American College Health. 2022;0(0):1-4. doi:10.1080/07448481.2022.2066976
3. Dyson K, Brown SP, May S, et al. International variation in survival after out-of-hospital cardiac arrest: a validation study of the Utstein template. Resuscitation. 2019;138:168-181. doi:10.1016/j.resuscitation.2019.03.018
4. Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63-81. doi:10.1161/CIRCOUTCOMES.109.889576
5. Riggs M, Franklin R, Saylany L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: A systematic review. Resuscitation. 2019;138:259-272. doi:10.1016/j.resuscitation.2019.03.019
6. Berg RA, Hemphill R, Abella BS, et al. Part 5: adult basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18_suppl_3). doi:10.1161/CIRCULATIONAHA.110.970939
7. Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002;105(5):645-649. doi:10.1161/hc0502.102963
8. Hands only CPR. cpr.heart.org. Accessed March 10, 2023. https://cpr.heart.org/en/cpr-courses-and-kits/hands-only-cpr
9. Bobrow BJ, Vadeboncoeur TF, Spaite DW, et al. The effectiveness of ultrabrief and brief educational videos for training lay responders in hands-only cardiopulmonary resuscitation: implications for the future of citizen cardiopulmonary resuscitation training. Circ: Cardiovascular Quality and Outcomes. 2011;4(2):220-226. doi:10.1161/CIRCOUTCOMES.110.959353
10. Panchal AR, Meziab O, Stolz U, et al. The impact of ultra-brief chest compression-only CPR video training on responsiveness, compression rate, and hands-off time interval among bystanders in a shopping mall. Resuscitation. 2014;85(9):1287-1290. doi:10.1016/j.resuscitation.2014.06.013
11. Anderson KL, Niknam K, Laufman L, Sebok-Syer SS, Andrabi S. Multi-community cardiopulmonary resuscitation education by medical students. Cureus. 12(6):e8647. doi:10.7759/cureus.8647
12. Bandura A. Self-efficacy mechanism in human agency. American Psychologist. 1982;37. https://psycnet-apa-org.proxy.library.upenn.edu/fulltext/1982-25814-001.pdf
13. Ro YS, Shin SD, Song KJ, et al. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016;102:17-24. doi:10.1016/j.resuscitation.2016.02.004
14. Fisher J, Ray A, Savett SC, Milliron ME, Koenig GJ. Collegiate-based emergency medical services (EMS): a survey of EMS systems on college campuses. Prehospital and Disaster Medicine. 2006;21(2):91-96. doi:10.1017/S1049023X00003411
15. Barry D. Do Not Use Averages with Likert Scale Data. Accessed March 30, 2023. https://bookdown.org/Rmadillo/likert/
16. Larose D. Chapter 14: Nonparametric Tests. In: Discovering Statistics. 3rd ed. W. H. Freeman. http://bcs.whfreeman.com/webpub/statistics/DiscoStat3e/Companion_Chapter/Larose_3e_Online_ch14_hires.pdf
17. Out-of-hospital chain of survival. cpr.heart.org. Accessed March 10, 2023. https://cpr.heart.org/en/resources/cpr-facts-and-stats/out-of-hospital-chain-of-survival
18. Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(6):596-601. doi:10.1197/j.aem.2005.12.021
19. Ornato JP, Hallagan LF, McMahan SB, Peeples EH, Rostafinski AG. Attitudes of BCLS instructors about mouth-to-mouth resuscitation during the AIDS epidemic. Ann Emerg Med. 1990;19(2):151-156. doi:10.1016/s0196-0644(05)81800-1
20. Cabrini L, Biondi-Zoccai G, Landoni G, et al. Bystander-initiated chest compression-only CPR is better than standard CPR in out-of-hospital cardiac arrest. HSR Proc Intensive Care Cardiovasc Anesth. 2010;2(4):279-285. Accessed March 10, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3484593/
21. Ong MEH, Ng FSP, Anushia P, et al. Comparison of chest compression only and standard cardiopulmonary resuscitation for out-of-hospital cardiac arrest in Singapore. Resuscitation. 2008;78(2):119-126. doi:10.1016/j.resuscitation.2008.03.012
22. Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116(25):2908-2912. doi:10.1161/CIRCULATIONAHA.107.710194
23. CPR in schools legislation map. cpr.heart.org. Accessed March 10, 2023. https://cpr.heart.org/en/training-programs/community-programs/cpr-in-schools/cpr-in-schools-legislation-map
24. Brown LE, Lynes C, Carroll T, Halperin H. CPR instruction in U.S. high schools. Journal of the American College of Cardiology. 2017;70(21):2688-2695. doi:10.1016/j.jacc.2017.09.1101
25. Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74(3):476-486. doi:10.1016/j.resuscitation.2007.01.030
26. Broomfield R. A quasi-experimental research to investigate the retention of basic cardiopulmonary resuscitation skills and knowledge by qualified nurses following a course in professional development. J Adv Nurs. 1996;23(5):1016-1023. doi:10.1111/j.1365-2648.1996.tb00084.
Author & Article Information
Junwon Kim, EMT-B is a rising senior at the University of Pennsylvania graduating with a BA in Biochemistry and MS in Chemistry and is the Community Outreach Officer of the Penn Medical Emergency Response Team. Max Yang, EMT-B is a rising senior graduating with a BA in Sociology at the University of Pennsylvania and is Chief of the Penn Medical Emergency Response Team. Akinkunmi Adio, EMT-B is a sophomore graduating with a BA in Neuroscience at the University of Pennsylvania and CPR Officer of the Penn Medical Emergency Response Team. Victor Tsao, EMT-B is a sophomore graduating with a BA in Biology and a BA in the History of Art at the University of Pennsylvania and Community Outreach Officer of the Penn Medical Emergency Response Team. Aarthi Kaviyarasu, BS graduated with a BS in Psychology from Duke University and is a clinical research coordinator at the Center for Resuscitation Science in the Department of Emergency Medicine at the University of Pennsylvania. Benjamin S. Abella, MD, MPhil, is a Professor and Vice Chair for Research, Department of Emergency Medicine, and serves as Director of the Center for Resuscitation Science, devoted to CPR research and education. Joshua E. Glick, MD is an Assistant Professor, Department of Emergency Medicine, and Medical Director for the Penn Medical Emergency Response Team.
Author Affiliations: From University of Pennsylvania Medical Emergency Response Team – in Philadelphia, Pennsylvania (J.K., M.Y., A.A., V.T., J.G.). From University of Pennsylvania, Department of Emergency Medicine – in Philadelphia, Pennsylvania (A.K., B.A., J.G.). From University of Pennsylvania, Department of Emergency Medicine, Center for Resuscitation Science (A.K., B.A.) – in Philadelphia, Pennsylvania.
Address for Correspondence: Junwon Kim | Email: jkim0312@sas.upenn.edu
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors declared no conflicts of interest. The authors declared that they received funding from the University of Pennsylvania Undergraduate Assembly and Center for Resuscitation Science to support the training event.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received April 14, 2023; accepted for publication June 28, 2023
Published Online: Pending
Published in Print: Pending
Reviewer Information: In accordance with JCEMS editorial policy, Original Research manuscripts undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2023 Kim, Yang, Adio, Tsao, Kaviyarasu, Abella, & Glick. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: Pending











