Due to the critical, short-term nature of emergency medical treatment, many emergency medical services (EMS) personnel currently do not have adequate resources for patients suffering from acute or chronic mental health complaints. In the United States, nearly 1 in 5 adults suffer from a mental illness within their lifetimes, suggesting the importance of regularly evaluating mental wellness during an emergency medical technician (EMT)’s assessment.1
In California, lack of or insufficient treatment among patients suffering from mental health conditions is unfortunately common. According to the 2018 California Health Care Almanac, over 50% of patients who have mental health disorders go untreated, regardless of whether or not they have insurance.2 At the college undergraduate level, it is clear that untreated mental illness is incredibly pervasive.3 College students experience unique stressors, including increased workload, interpersonal relationships, and making decisions independently. Because roughly 75% of lifetime cases of psychiatric disorders manifest by age 24 and recent years have seen a notable increase in reported mental health symptoms among college students, it is essential for universities to create and implement support systems for students’ experiencing mental health crises.4 The increase in symptoms of mental health conditions and demand for mental health services also has significant implications for collegiate-based emergency medical organizations, who are tasked with responding to medical emergencies for their fellow classmates. Collegiate EMS programs have grown with an impressive rate over the past twenty years, yet there remains a lack of research and evidence based guidelines surrounding how we can best serve college students in need of behavioral health services.Within the Emergency Medical Services of USC (EMSC), a student-run event-based volunteer EMT program at the University of Southern California, our staff have witnessed multiple occurrences of patients self-diagnosing and self-treating severe psychiatric conditions–like depression, anxiety, and ADHD. Because we only treat our patients on a short-term stand-by basis, and typically for chief complaints unrelated to their complex mental health medical histories, there appears to be little to do to encourage them to seek long term care. Exasperating this issue is the fact that while many organizations exist to help patients with severe mental illness (SMI), low treatment rates indicate that lack of awareness and social stigma are two of the biggest barriers to treatment for these populations.5
The problems of awareness and stigma can first be witnessed and potentially addressed at the EMT level. By training first responders to not only navigate SMI calls but to also provide information on treatment options and available resources, providers can work to increase the rate of treatment for those suffering from SMIs through contact at what is often the initial step of a care cascade. In addition to this, by providing this information, EMTs would effectively initiate patient-centered care methods, which studies suggest is crucial in treating individuals with mental illness, especially for those with serious mental illnesses who have much higher dropouts and attrition rates from ongoing treatment.6
The first step in improving the EMS response towards SMI cases is to educate first responders on identifying cases where mental health plays a role in the patient’s situation. Due to stigmas clouding mental health (i.e. lack of understanding by family, friends, etc., feelings of isolation and shame, reluctance to ask for help/seek treatment), it might not always be immediately clear that a call pertains to a mental health crisis. However, by forming context around the patient’s situation through questions, EMTs can elucidate the mental health components to a patient’s situation. In this review, we evaluate existing resources, their potential impact on and integration into EMSC and other collegiate EMS programs, barriers to treatment, and next steps for mental health integration and awareness in EMS.
The College Demographic & SDOH
The link between an individual’s social environment and their health has long been recognized within the domains of public health and medical care systems. A mounting body of research suggests that persistent disparities in health status can be traced to largely inescapable underlying factors including race, ethnicity, age, income level, education level, sexual orientation, geographic location, interpersonal, family, and community dynamics, housing quality, social support, employment opportunities, work and/or school conditions and other factors contributing to an individual’s built environment.7 These underlying factors, termed social determinants of health (SDOH), are defined by the World Health Organization (WHO) as “conditions in which people are born, grow, live, work, and age…circumstances [which] are shaped by the distribution of money, power and resources at global, national and local levels.”8 The relationship between SDOH and health status has become especially evident during the COVID-19 pandemic, which has exacerbated the nation’s systemic inequalities and disproportionately affected racial minorities and low-income communities.9
The U.S. fee-for-service health care system has historically struggled to integrate public health and preventive services into their framework, largely because they had little incentive to do so.10 The consequences of these social determinants are starkly evident within emergency medical services (EMS), where front-line providers are tasked to treat the patient’s chief complaint, but are often unable to address upstream issues of homelessness, addiction, food insecurity, racism, and more–which are some of the main predictors of a patient’s health outcomes.
College environments and early adulthood bring about significant changes that impact students’ SDOH. One manifestation of these changes is the disproportionately high rate of suicide. Between 2007 and 2017, the rate of death by suicide among individuals aged 15 to 24 had increased by 57%.11 As of 2018, suicide was the second leading cause of death for the same age group.12 Similarly, rates of suicide ideation, planning, and attempt are higher among adults aged 18 to 25 compared to older adults.13 In 2015, a national survey conducted across 108 institutions found that approximately 1 in 5 undergraduate students had considered suicide, 1 in 10 had made an attempt, and nearly 1 in 5 reported self-harm.14,15 This disparity has likely been worsened by COVID-19. Many students are now living out-of-state due to stay-home orders and experience decreased access to campus therapists since licensure laws prohibit or limit practice across state borders.16
While medical providers increasingly recognize the need to address SDOH in patient care, the process of implementation remains less clear, especially as it pertains to EMS providers, who are often limited by a lack of time and resources. There is a clear need for EMS training programs and employers to develop guidelines on the best practices to identify and address social determinants in prehospital care.17 In the interim to the creation and implementation of such guidelines, many emergency departments and some community paramedicine programs have begun to use their expertise and leadership to develop screening and referral practices to bridge the divide between emergency services and the social determinants of health.18 After a review of EMS initiatives to implement social determinants into their care framework, we defined programs as successful if their results demonstrated significant increases in post-training gains across domains related to SDOH knowledge and attitudes and/or skills pertaining to mental health de-escalation and referral, as compared to baseline assessments. From this classification, we observed that collegiate EMS organizations who had been successful in creating programs specifically to response to mental health complaints on campus shared the following three elements: 1) standardized screening guidelines 2) integrated referral practices and 3) community partnerships. Accordingly, we recommend collegiate EMS programs to take the following measures to better integrate emergency services and social determinants of health into the acute treatment of complex mental and physical health complaints:
1. Standardized Screening
While clinical guidelines increasingly recommend the SDOH be captured and recorded, there is a lack of standardized screening tools and processes. A standardized screening process is essential to allow different players across healthcare and social service systems to communicate effectively and have a common frame of reference. Prehospital providers can implement the Question, Persuade, and Refer (QPR) Screening Tool into their secondary assessment and can use the results to inform patients’ treatment plans and make referrals to community services.
Our Intervention: Question, Persuade, Refer (QPR)
To improve screening for mental illness, we recommend collegiate EMS programs incorporate gatekeeper training to improve suicide prevention, especially given that an increase in self-diagnosed and self-treated mental illnesses is likely when campuses open.19 Collegiate EMS must be prepared to provide adequate care within its scope, and gatekeeper training can empower it to do so.
Gatekeeper training is a nationally recognized suicide prevention program. In one or two hours, one learns to identify at-risk individuals and refer them to counseling and support services. Although there is no prerequisite education for the training, an ideal gatekeeper is “strategically positioned” to recognize and refer individuals.20 Collegiate EMTs are ideal candidates: not only do they have high proximity and familiarity with fellow students, but they are also likely to encounter mental health crises on calls, or to notice warning signs of mental illness during secondary assessment.
In addition, principles of gatekeeper training align with those of a well-established EMS procedure. Question, Persuade, and Refer (QPR) is the most widely used gatekeeper program in the United States and is recommended by the Substance Abuse and Mental Health Services Administration (SAMHSA). QPR shares procedural similarities with cardiopulmonary resuscitation (CPR). At their cores, both aim to increase a patient’s chances of survival by prioritizing early recognition and intervention.20 Although CPR does have a more demonstrable effect on patient survival, QPR education has been proven to significantly improve attitudes, subjective norms, and perceived behavioural control regarding suicide intervention.21 QPR training for EMTs can serve as an extension to their life-saving skills, allowing them to remain calm and rely on a standardized procedure when responding to mental health crises.
The University of Southern California offers micro-grant applications to recognized student organizations through the student health center’s wellness program. Applying such a microgrant to the QPR training of EMTs that serve our student population invests resources back into our community to promote the long-term wellbeing of our student population and the ability of our EMTs to respond to such calls effectively. Fortunately, such funding is not limited to the University of Southern California. Most colleges and universities across the nation provide similar application-based funding to recognized student organizations through their undergraduate government bodies. At the minority of institutions that may not have such robust funding, organization-led crowd fundraising efforts through GoFundMe or alternative methods (bake sales, member dues) could also provide the necessary funding for such a program.
Limitations: The major limitations regarding QPR in EMS involve the period of time that training remains effective. Previous studies indicate that QPR training was effective in increasing immediate knowledge, attitudes, and skills to prevent suicide; however, these effects were only studied in a short-term time frame.22 Without scheduled refresher courses, the knowledge gained from QPR training can fade and cause providers to be less confident in approaching mental health emergiencies. The period of time in which training remains effective varys from provider to provider, but it has been shown that in two-year post-training follow ups, EMS providers felt significantly less confident, knowledgeable, and prepared to deal with mental health crises.23 Further research is needed on the efficacy of long-term and systemic efforts to integrate QPR into EMS. Regardless, we recommend QPR training–it is an evidence-based intervention that provides sorely needed skills to address high rates of suicides on college campuses. Furthermore, EMS on the collegiate level might be more conducive to continuous QPR refreshers than traditional EMS organizational structures. Because new students join collegiate EMS organizations every year, there is a constant need for training. By involving all crew members in this training, collegiate EMS organizations can prevent knowledge loss and provide consistent, high-quality care to the populations they serve.
Although there is a paucity of research on QPR with regard to collegiate EMS, there is evidence to support its efficacy in similar settings and populations. QPR in a college environment was effective in increasing immediate knowledge, attitudes, and skills to prevent suicide, as demonstrated through a short-term study conducted with residence advisors.22 A methodologically similar two-year study supports short and long-term results with gatekeepers who work with youth.23 Further research is needed on long-term and systemic efforts to integrate QPR. Regardless, we recommend QPR training–it is an evidence-based intervention that is theoretically a match for EMTs, and provides sorely needed skills to address high rates of suicides on college campuses.
2. Integrated Referral Practices
To bolster the presence of integrated referral practices during collegiate EMS calls, it is imperative that collegiate EMS programs work with their university’s health departments to identify mental health resources for students of various backgrounds, ranging from free group therapy options to individual therapy and more.
Our intervention: Student-Health Center Partnership
It is important that we recognize our limited role in the long-term care of patients, as in-field stand-by EMTs. Unlike a majority of other collegiate EMS organizations, we are not involved in routine calls or patient transport. As such, the time and resources we have to provide care to patients needing longitudinal support can often be inadequate. Thus, it becomes vital to build a strong relationship with long-term mental health care resources in our community. The most accessible and advertised resource for our student population is the Engemann Student Health Center, located on the larger of our two campuses. The staff continually implement quality improvements to stretch their resources in service of our student population. Their preference is to screen and refer students, rather than offer long term care within their own facilities–a result of the immense demand for care among our student population of over 20,000. Reasonably, a student not immediately referred to an Emergency Department after leaving our care would likely be referred to Engemann. But, a gap exists in care-seeking behavior for students whose mental health concerns are not urgent enough to require immediate continued care.24
As such, our EMS agency reached out to the student health staff at Engemann to build a partnership for direct referrals, with the general guidelines of consent and HIPAA compliance preserved in all activities. This serves to eliminate the barrier of actively needing to seek care multiple times (at least once from our EMTs, then again for continuity of care), and feeds well into a potential recipient of our QPR program. When referring students to further care, compliance improves when care is accessible, both in location and familiarity.25 For our specific resource-based intervention, we extrapolate the broad value of connecting EMS to continued care whenever possible. As such, we encourage other collegiate EMS programs to likewise seek longitudinal partnership with primary care and urgent care providers at their institutions’ student health centers or other nearby healthcare institutions.
Limitations: At the time of publication, we have not yet received a formal response from a representative at the Engemann student health center about formally implementing a direct referral program for patients we respond to on shift experiencing a mental health crisis but we remain open to partnership and continue to explore other community-based options for referrals to continued mental health care. While EMSC already has a working relationship with a Health Promotion Specialist at Engemann who advises us about crisis de-escalation on shift and wellness practices for our student EMTs, we believe there remains a gap in the transfer of care between the immediate mental health services we provide on shift and longer-term mental health treatment offered at Engemann. Expanding our partnership with Engemann to include direct referrals for patients experiencing a mental health crisis would better address the upstream factors leading to the emergent situation. As EMSC and other collegiate EMS programs become more deeply integrated into university’s emergency response systems, collaboration both within and between existing institutions is necessary to develop proactive solutions to best promote the health and safety of the students these institutions serve.
3. Community Partnerships
Collegiate EMS programs can assist in expanding awareness of existing resources through building partnerships with the university’s mental health programs, local mental health clinics, and on-campus, student-run organizations. Once mental health resources are identified for a broad array of student populations, covering various combinations of SDOH, collegiate EMS programs can package these resources into small infographics, brochures, etc. that may be handed out to all patients during calls. Furthermore, after the standardized screening in step 1, the EMS provider may have a better understanding of which specific mental ailment(s) the patient may be suffering from. At this point, the provider may be able to provide more specific, premade resources to the patient so they are able to seek treatment beyond the short-term treatment that the provider offers.
Our Intervention: Patient Resource Card
As an agency, we implemented a shift data review and classification process in the Spring of 2019 to develop evidence-based quality improvement strategies. The process involved a confidential review of shift employee records to code data by call type, frequency, partner agency dynamics, and extraordinary circumstances. A manual inductive approach was used to analyze and code the aggregated qualitative and quantitative information to identify recurring trends. This data was then used to facilitate actionable decision making in our organization, whether in continued training or mediated debriefs with staff. We rapidly noticed an alarming prevalence of mental health concerns (both chief and secondary) in our call logs. In formal post-shift debriefs, our EMTs often noted a sense of helplessness when attempting to offer further care resources to such patients, only vaguely referencing our student health center and national resources while on scene. EMTs receive very little mandated training on mental health; further, they rarely receive any training at all from employers on local mental health resources for patients. The nature of our collegiate EMS program involves high turnover, which makes changes to foundational protocol more effective than cohort training alone. After implementing a dedicated psychiatric emergencies lecture into our skills training sessions curriculum, we decided to pursue broader protocol reform to ensure a lasting impact on EMT preparedness to handle calls that are psychiatric in nature, whether emergent or not.
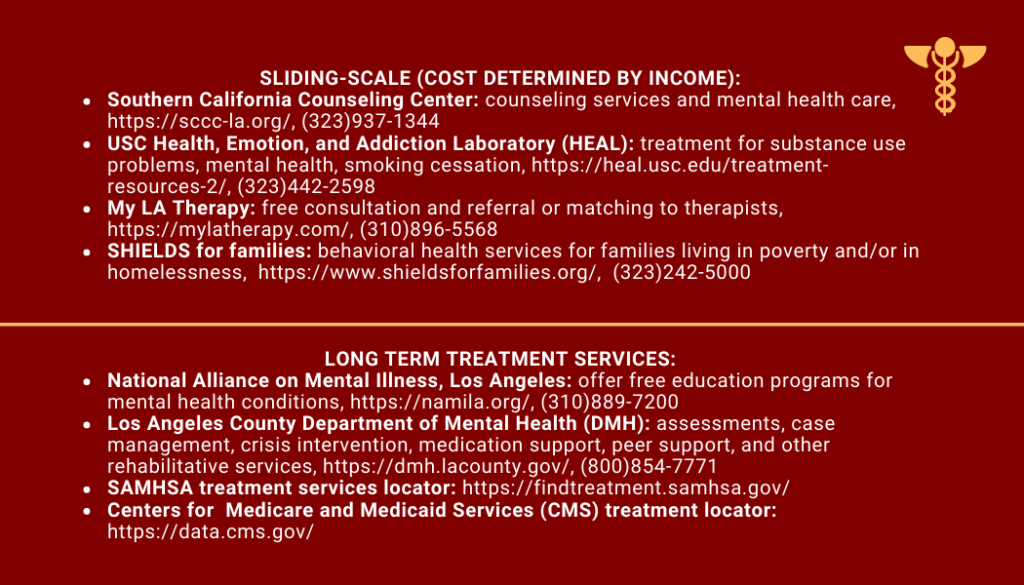
Thus, we added a gear item to our oxygen bags, alongside our clipboards and patient care reports: a mental wellness resource card. The card is discreet in size and includes references to campus-specific, community-specific, cost-specific, and national/remote care. Given the nature of the COVID-19 pandemic and its resulting halt of recreational events which our organization traditionally staffs, we have not yet received real-time feedback from our community as to the efficacy of the resource card. The card, however, is designed to be reevaluated as necessary by EMSC’s Director of Internal Relations (a fairly new role, only proposed in Spring 2019), who is responsible for staff wellness, personnel logistics, and conflict management. As the nature of internal affairs management is vastly different depending on collegiate EMS program size and resource capacity, we recommend organizations seek out a distribution of responsibility (i.e. tasking this to student volunteers versus outsourcing to credentialed professionals) best suited to their own needs.
Figure 1: Our most recent card template, revised in Fall
2020 (front)
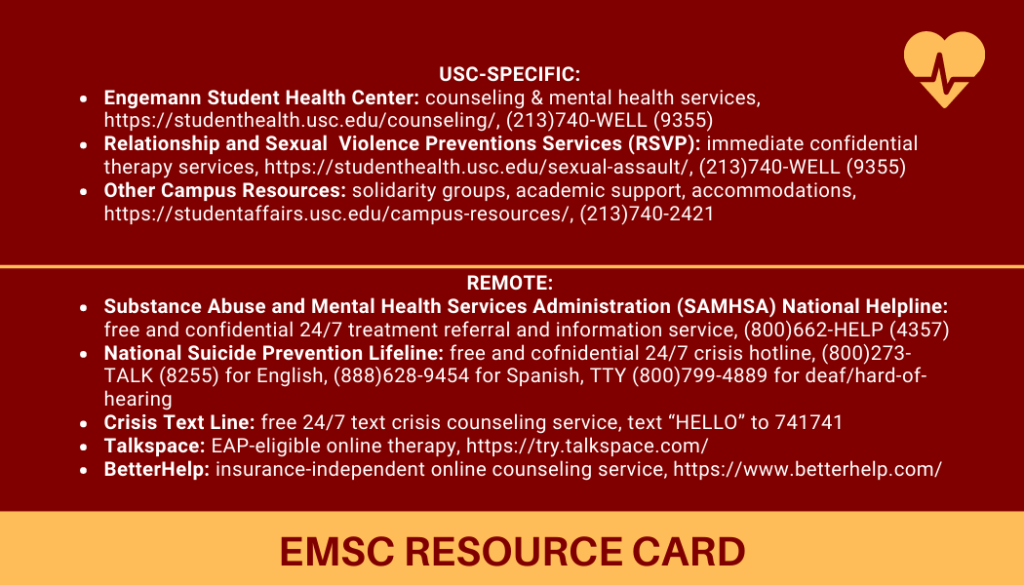
Figure 2: Our most recent card template, revised in Fall
2020 (back)
Limitations: In order to create sustainable partnerships with local resources, we promote going beyond raising awareness to the formation of concrete and fluid partnerships. By working with the university’s mental health programs and local mental health clinics, collegiate EMS programs will first identify the most important resources to build awareness about. Then, by working with on-campus, student-run organizations, collegiate EMS programs can provide brief presentations on existing resources. Furthermore, collegiate EMS programs may be able to build websites with tools (such as brief quizzes or surveys) to walk students through which mental health resource(s) may be best for them during a specific crisis. By expanding awareness of such resources through presentations and partnerships with on-campus student-run organizations and personalizing them to the student’s needs with quizzes and/or surveys, collegiate EMS programs would be able to greatly demystify the daunting steps required to seek mental health resources.
Conclusion
Prehospital providers work within the community setting and are well positioned to connect medical care with social and community resources. As students themselves, collegiate EMS providers are uniquely situated to acutely understand the social factors impacting their classmates and how to compassionately refer them to relevant community services and resources. By tailoring the proposed intervention to best suit the needs of the receiving demographic, EMS agencies can best equip their staff to respond appropriately and effectively to complex calls, especially those involving mental health complaints.
References
- Mental illness. NIMH. November 2, 2020. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml. Accessed December 19, 2020.
- Holt W. Mental health in California. CHCF. March 28, 2018. https://www.chcf.org/publication/2018-edition-mental-health-ca-for-too-many-care-not-there/#:~:text=Mental%20health%20disorders%20are%20among,carry%20out%20major%20life%20activities. Accessed December 21, 2020.
- Blanco C, Okuda M, Wright C, et al. Mental health of college students and their non–college-attending peers. Arch Gen Psychiatry. 2008;65(12):1429-1437. doi:10.1001/archpsyc.65.12.1429
- Lattie EG, Lipson SK, Eisenberg D. Technology and college student mental health: challenges and opportunities. Front Psychiatry. 2019;10(246). doi: 10.3389/fpsyt.2019.00246
- Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare. Healthc Manage Forum. 2017;30(2):111-116. doi:10.1177/0840470416679413
- Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry. 2015;39:503-511. https://dx.doi.org/10.1007%2Fs40596-014-0205-9
- Social determinants of health. USDHHS. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Accessed December 19, 2020.
- Social determinants of health. WHO. https://www.who.int/gender-equity-rights/understanding/sdh-definition/en/. Accessed December 19, 2020.
- COVID-19: health equity considerations and racial and ethnic minority groups. CDC. July 24, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed December 19, 2020.
- Litteken C, Sale E. Long-term effectiveness of the Question, Persuade, Refer (QPR) suicide prevention gatekeeper training program: lessons from Missouri. Community Men Health J. 2017;54(3):282-292. https://doi.org/10.1007/s10597-017-0158-z
- Lurie N, Fremont A. Building bridges between medical care and public health. JAMA. 2009;302(1):84-90. doi:10.1001/jama.2009.959
- Curtin SC, Heron M. Death rates due to suicide and homicide among persons aged 10-24: United States, 2000-2017. Centers for Disease Control and Prevention. October 17, 2019. https://www.cdc.gov/nchs/products/databriefs/db352.htm. Accessed December 13, 2020.
- Suicide. NIMH. https://www.nimh.nih.gov/health/statistics/suicide.shtml. Accessed December 13, 2020.
- Piscopo K, Lipari RN, Cooney J, Glasheen C. Suicidal thoughts and behavior among adults: results from the 2015 national survey on drug use and health. SAMHSA. 2016. https://www.samhsa.gov/data/sites/default/files/NSDUH-DR-FFR3-2015/NSDUH-DR-FFR3-2015.htm. Accessed December 19, 2020.
- Liu CH, Stevens C, Wong SH, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress and Anxiety. 2018;36(1):8-17. https://doi.org/10.1002/da.22830
- Lumpkin L. College students count on their schools for mental-health help, but now many can’t get it. The Washington Post. June 7, 2020. https://www.washingtonpost.com/local/education/college-students-count-on-their-schools-for-mental-health-help-but-now-many-cant-get-it/2020/05/28/e6f6e710-8b2b-11ea-ac8a-fe9b8088e101_story.html. Accessed December 13, 2020.
- Axelson DJ, Stull MJ, Coates WC. Social determinants of health: a missing link in emergency medicine training. AEM Education and Training. 2017;2(1):66-68. doi:10.1002/aet2.10056
- Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39(1). doi:10.1186/s40985-018-0094-7
- What is QPR? QPR Institute. https://qprinstitute.com/about-qpr. Accessed December 13, 2020.
- Mitchell SL, Kader M, Darrow SA, Haggerty MZ, Keating NL. Evaluating Question, Persuade, Refer (QPR) suicide prevention training in a college setting. J Coll Student Psychotherapy. 2013;27(2):138-148. https://doi.org/10.1080/87568225.2013.766109
- Aldrich RS, Wilde J, Miller E. The effectiveness of QPR suicide prevention training. Health Education Journal. 2018;77(8):964-977. doi:10.1177/0017896918786009
- Tompkins TL, Witt J. The short-term effectiveness of a suicide prevention gatekeeper training program in a college setting with residence life advisers. J Prim Prev. 2009;30(2):131-149. https://doi.org/10.1007/s10935-009-0171-2
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2009;46(1):3-10. https://doi.org/10.1016/j.jadohealth.2009.08.008
- Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update [published correction appears in World Psychiatry. 2016 Jun;15(2):189]. World Psychiatry. 2016;15(1):13-20. doi:10.1002/wps.20306
Author & Article Information
Inaya Riaz, BA, EMT completed her B.A. in Medical Anthropology in 2021 and is working towards completion of a M.S. in Global Medicine, both from the University of Southern California. She served as an EMT and a board member for EMSC from 2018 through 2021. Outside of USC, she has worked in ambulance and disaster cycle positions in her community, and continues to work full time with an interdisciplinary street medicine team under the Los Angeles Department of Health Services, providing essential medical care to unhoused populations. Gal Lapid, EMT is a fourth-year student at the University of Southern California, a current candidate for a B.S. in Health Promotion and Disease Prevention and a Master of Public Health. She has served as an EMT since 2019 and a board member for EMSC since 2020. She has worked as an EMS Reserve on a Rescue Ambulance and currently works as a Public Policy intern at People Assisting The Homeless (PATH). Mihir Kumar, EMT is a fourth-year student at the University of Southern California, a current candidate for a B.S. in Human Biology and a B.A. in Economics. He was certified in the Summer of 2019 and has been a member of EMSC since the Fall of 2019. Ravi Trivedi, BS, BA, EMT, is a first-year medical student at the Western Michigan Homer Stryker MD. School of Medicine. He received a B.S. in Neuroscience and a B.A. in Economics from the University of Southern California in 2021. He was certified in the Summer of 2018 and has been a member of EMSC since the Fall of 2019. Sulley Park, EMT is a fourth-year student at the University of Southern California, a current candidate for a B.S. in Health Promotion and Disease Prevention. He was certified in the Fall of 2019 and has been a member of EMSC since the Spring of 2020.
Author Affiliations: From The Emergency Medical Services of the University of Southern California – in Los Angeles, CA (I.R., G.L., M.K., R.T., S.P.).
Address for Correspondence: Inaya Riaz, BA, EMT | Email: iriaz@usc.edu
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors declared that they have no conflicts of interest. All authors declared that they did not receive funding to conduct the research and/or writing associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received December 23, 2020; accepted for publication August 5, 2021.
Published Online: October 31, 2021
Published in Print: October 31, 2021 (Volume 4: Issue 2)
Reviewer Information: In accordance with JCEMS editorial policy, Advice and Practice manuscripts are reviewed by the JCEMS Editorial Board and, as needed, independent reviewers. JCEMS thanks the Editorial Board members and independent reviewers who contributed to the review of this work.
Copyright: © 2021 Riaz, Lapid, Kumar, Trivedi & Park. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2021.04.02.01











