Abstract
Background: Collegiate emergency medical technicians (EMTs) often encounter patients with uncomplicated alcohol intoxication who may refuse transport to an emergency department (ED), but research lacks on the influence of bystander intervention on an EMT’s decision to let a patient refuse transport. Objective: We investigated how bystander intervention influences transport decisions in cases of alcohol intoxication at a small college in New York State. Methods: Data were collected from prehospital care reports (PCRs) archived by the college’s emergency medical services between 2014 and 2018. Included data were collected on alcohol intoxication cases (n = 190) and categorized by transport decision, nature of bystander intervention, and patient’s sex. Interactions between bystander intervention and transport decision were assessed by calculation of relative risks of ED transport and creation of a loglinear model. Results: Bystanders were present in a majority of cases, and a majority of bystanders offered to provide care following refusal of transport. Bystander presence was not associated with a significant difference in transport decision. However, when bystanders were present, offering care was associated with a 73% reduction in ED transport. Conclusions: Bystander care was found to be associated with a decreased relative risk of ED transport. However, documentation of bystander intervention in PCRs was often ambiguous. We highlight the need for better bystander intervention documentation in PCRs to improve research on this topic.
Introduction
Bystanders are often the primary actors in recognizing an emergency and activating emergency medical services (EMS).1-2 Their positive role has been extensively studied in cases of initiating cardiopulmonary resuscitation and intervening in potential sexual assault.1-3 Alcohol-related emergencies have the potential to benefit similarly from bystander intervention, as college students frequently seek help during alcohol emergencies.4 Meanwhile, underage binge drinking remains common among undergraduate college students.5-7 Because fear of legal or financial consequences may prevent students from seeking help, several college administrations have established amnesty policies for cases of alcohol emergencies, encouraging students to call for EMS.4, 8-9 These amnesty policies have been associated with an increase in bystanders calling for emergency services during a crisis.8 Additionally, research suggests that implementing educational programs to recognize the signs and symptoms of an emergency and perform basic safety measures tends to increase rates of bystander intervention across college campuses nationwide.3, 5-12 However, the literature on the practical implications of bystander intervention still lacks research with regard to alcohol-related emergencies on college campuses.
EMS providers are often faced with the difficult decision of whether an intoxicated patient requires transport to an emergency department (ED), transport to a detoxification facility, or may be allowed to refuse further medical treatment and transport. These decisions have an important role in reducing the burden on EDs across the country, as inebriated patients incur $900 million in hospital charges annually.13-14 In response to this issue, several communities have created detoxification facilities which provide limited medical care to non-critical patients.13-15Finally, in many circumstances, patients have the ability to consent and express a desire to refuse further medical care and transport. In these cases, providers may play a notable role in discouraging this decision if they feel further care is warranted. Therefore, the outcome of an EMS interaction with an intoxicated patient is highly variable. While past reports have attempted to identify assessment criteria for triaging intoxicated patients by physical and mental presentation, past medical history, vital signs, and the provider’s informed judgement, few reliable predictors of clinical outcomes have been identified.13-17
This study assessed the influence of bystander intervention on collegiate EMS transport decisions in alcohol intoxication cases. Considering that bystanders may be willing to take basic measures to ensure the safety of a patient, such as caring for them or providing them transport to further care facilities,4, 8-10 we hypothesized that final transport decisions may be related to either bystander presence at the scene or their willingness to provide care for patients refusing transport.
Methods
Study design
We performed a retrospective cohort study. Data were collected from handwritten paper prehospital care reports (PCRs) maintained by a collegiate EMS agency in New York State.18 PCRs were reviewed and considered for inclusion for every patient during the academic semesters from the fall of 2014 to the spring of 2018. The study was approved by the Bard College Institutional Review Board. Due to minimal risk posed to patients and the retrospective study design, it was determined that the study warranted a waiver of informed consent.
PCR selection and interpretation
Two inclusion criteria marked PCRs for selection: 1) alcohol use listed as a presenting problem, or 2) reference within the PCR narrative to the amount or type of alcohol ingested by the patient. PCRs that did not meet inclusion criteria were excluded from the study.
We defined any non-EMS person present at the scene and actively willing to contribute to the patient’s care as a “bystander.” While not necessary, bystanders were often people who already knew the patient prior to the incident, such as family, friends, roommates, and colleagues. Although there is no specific requirement in the standard PCR format to document bystander presence, EMS interactions with bystanders are typically included in the narrative portion of the PCR. Therefore, included PCRs were classified by whether or not bystander presence was documented. Among cases in which bystander presence was documented, PCRs were further classified by whether or not it was documented that bystanders were willing to care for the patient if they refused transport. This care may have included looking after the patient, sitting with the patient, providing private transport to further care, and/or offering to call for EMS again as needed.
Transport decisions were documented with a numerical disposition code at the bottom of the PCR, either 004 for ambulance transport to the ED or 005 for refusal of further medical care and transport. Outcome data was coded as either “Transport” or “No Transport.” In addition, patient sex was recorded as either “Male” or “Female.” The general terms used to describe the data were chosen to de-identify the subjects as much as possible. For the same reason, we did not record data on other factors used to determine transport decision, such as presence of trauma or use of other drugs in addition to alcohol.
Statistical analyses
Relative risks (RRs) and 95% confidence intervals (CIs) were determined for the associations between the three predictor variables (bystander presence, bystander care, and patient sex) and the outcome variable of transport decision.
Loglinear models using a Poisson distribution were employed to further analyze the interactions between categorical data variables.19-20 The best-fit loglinear model to account for the interactions between the variables was found using a likelihood ratio test to assess deviance from a saturated model that perfectly fit the data (significance value calculated on chi-squared distribution).19-20 The specific significant interactions between the modeled variables were determined through a three-way analysis of variance followed by a Tukey honest significant difference (HSD) post-hoc test.19-20
The calculations for RRs and CIs, loglinear models, statistical tests, and figures were done in RStudio (RStudio Team (2018). RStudio: Integrated Development for R. RStudio, Inc., Boston, MA, URL http://www.rstudio.com/, desktop version 1.2.1335), using the epiR package (version 1.0-4) for RRs and CIs and ggplot2 (version 3.2.1).
Results
During the academic years of 2014 through 2018, the collegiate EMS agency was dispatched to 190 cases of alcohol intoxication. These account for nearly one fifth (18%) of the total calls responded to during that period. Among alcohol intoxication cases, 82% included bystander participation (Table 1). According to PCR narratives, 72% of bystanders offered to care for a patient following their refusal of transport (Table 1). In addition, 57% of patients were female and 43% were male (Table 1).
Table 1: Basic characteristics of all alcohol-involved cases at a New York collegiate EMS agency, 2014-18
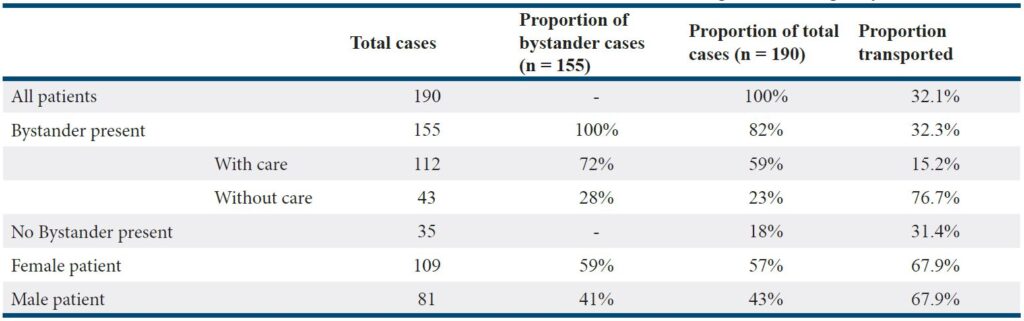
As shown in Table 1, 32% of alcohol intoxication patients were transported. Bystander presence vs. absence was not associated with a significant difference in risk of transport (p = 0.92) (Figure 1). However, among cases with bystanders present, transport risk was significantly lower when bystanders offered care (RR = 0.27, 95% CI [0.17, 0.43], p < 0.001) (Figure 1). In the majority of cases involving bystanders that did not offer care, the patient was transported to the ED (Table 1). Risk of transport did not vary significantly by patient sex regardless of bystander status (Figure 1).
Figure 1: Bystander care lowers the relative risk of patient transport to the emergency department
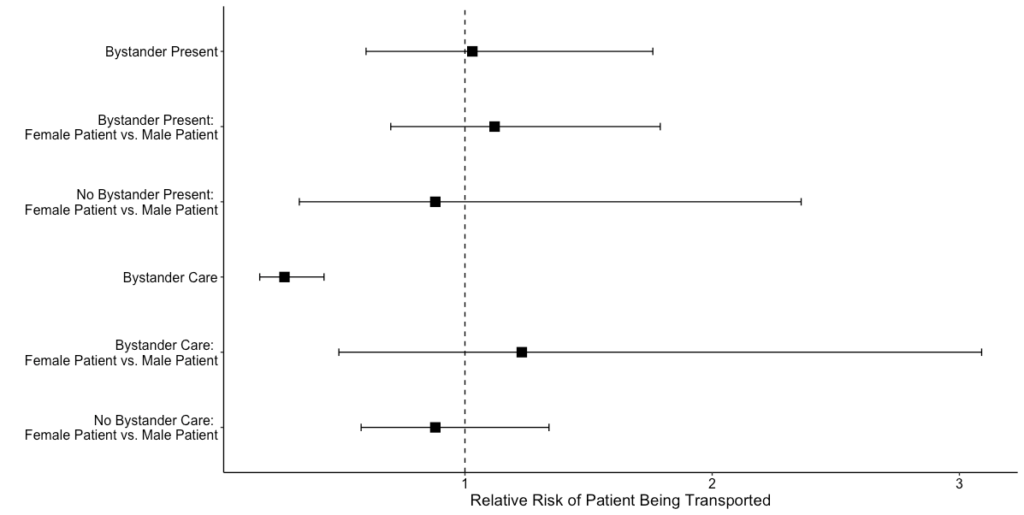
To further assess the interactions between bystander care and transport decision, we computed the frequencies of coincidences between the variables and generated loglinear models of the data.19 We found that a homogenous association model, which accounted for all pairwise interactions between the variables and their frequencies, fit the data as well as a saturated model that accounted for all interactions between the variables to the frequencies (likelihood ratio test, Deviance = 0.096, degrees of freedom = 2, p = 0.95). With the homogenous association model, we found a significant difference between the type of bystander intervention and the transport decision (F(2, 2) = 30.33, p = 0.03). Post hoc tests only showed statistically significant differences in three scenarios: not transported cases between bystander presence and bystander care (p = 0.038), between transported cases without bystanders and not transported cases with bystander care (p = 0.047), and between not transported cases with and without bystander care (p = 0.045). Meanwhile, the effect of bystander intervention on transport decision did not differ much between sexes (p > 0.1 for all pairwise interactions), suggesting little bias on transport decisions made toward either sex.
Discussion
Alcohol intoxication cases were a common occurrence for the collegiate EMS agency during the period of study. Bystanders participated in the majority of these cases, and a majority of bystanders offered to care for the patient. Approximately one-third of alcohol intoxication patients were transported.
Our data suggest that bystanders willing to provide care were influential in EMS decisions to let an alcohol intoxication patient refuse transport. Although the relative risk of ED transport for most predictor variables neared 1, the risk of ED transport was reduced by 73% when a bystander offering care was present at the scene. Post hoc analysis of our pairwise interaction model also found that transport decisions in cases with bystander care differed significantly from cases without bystander care. It is therefore likely that transport decisions made by the collegiate EMS agency were affected by the presence of a caring bystander. Of note, the presence of a bystander at the scene regardless of caring status was not found to reduce the risk of ED transport. However, because only three of all modeled pairwise associations between transport decision and bystander intervention were significantly different, it is hard to speculate the implications of the apparent reduction in ED transport related to bystander care in other scenarios.
In accordance with the previous literature, our data show that the effect of bystander intervention on transport decision did not differ by patient sex.8 This may be due in part to widespread bystander intervention education for students and campus medical amnesty policies.8
Our results suggest that a bystander’s willingness to care for a patient can reduce the relative risk of transport to an ED. We speculate that this reduction might be related to the EMTs’ and the patient’s increased confidence that the patient will stay safe after EMS dismissal when a caring bystander is present.
Limitations
One challenge in conducting this study was that PCRs do not specifically require the documentation of bystander intervention.18 Therefore, it is probable that bystander presence or care was not documented in some cases, leading to a potential underestimation of the frequency of these events in our data. The inconsistency of bystander documentation also prevented a more detailed analysis. PCRs did not necessarily reveal the relationship of the bystander to the patient, so we could not assess differences in the influence of a family member, friend, roommate, or stranger on transport decisions. Also, while New York State protocols use the term “responsible adult” to describe someone who may care for a patient after refusal of EMS transport,17 there was not enough information in the PCRs to let us assess each bystander’s level of “responsibility.”
Our study did not consider several variables which may have informed interpretation of the results. These included several factors that may affect a transport decision following an alcohol intoxication call, such as the amount and type of alcohol consumed, signs of alcohol poisoning, the intake of illicit drugs, and presence of physical trauma. However, we judged that recording these factors would not be necessary as their incidence legally corresponds to a necessary transport to a hospital due to the established protocols in New York.17 Additionally, we could not assess patient outcomes following the final transport decision due to the prehospital nature of the archives.
Because we did not record patient names to comply with deidentification requirements, we were unable to determine if multiple PCRs referred to the same patient at the same event. For example, a patient may have initially been allowed to refuse further care and then required EMS intervention again due to worsening condition. Therefore, it is possible that our data contain instances of duplicated individuals.
Due to the textual nature of PCR narratives, interpretation of these narratives could potentially vary subjectively between observers. Consequently, our PCR interpretation process could have benefitted from an inter-rater reliability assessment.
Finally, this study was conducted in the specific environment of a small liberal arts college in New York State. Similar investigations in other collegiate and non-collegiate EMS settings are required to test the generalizability of the trends found.
Conclusion
Our data suggest that the presence of a caring bystander decreased the likelihood of transporting a patient with reported alcohol intoxication to an ED in a collegiate EMS setting. These decreases in likelihood were similar between male and female patients. Because of the trend shown in this retrospective study, it is important to raise awareness among collegiate EMS agencies about the potentially pivotal role that bystanders can play in a collegiate alcohol intoxication case.8-9 Bystanders may be a resource when transport is declined, but we recommend that EMTs keep protocols in mind and not bias their assessment of a patient solely due to the presence of a bystander at the scene.8, 17 We propose that future understanding of patient outcomes after EMS dismissal—either to a hospital or to a bystander—and better documentation of bystander intervention in PCRs may improve how EMTs make decisions for the patient’s best interest,8-9, 17 as well as further research in this topic by other collegiate EMS agencies.
Acknowledgements
We would like to acknowledge the mentorship of Bard College faculty members Helen Epstein, PhD, visiting professor of human rights and global public health, Arseny Khakhalin, PhD, assistant professor of biology, as well as the mentorship of Dr. Angela Cavanna, DO, and thank all members of the Bard College EMS team. The authors did not receive any funding sources or grants to conduct this research. The authors declare no conflicts of interest.
References
- Sayre Michael R., Berg Robert A., Cave Diana M., Page Richard L., Potts Jerald, White Roger D. Hands-Only (Compression-Only) Cardiopulmonary Resuscitation: A Call to Action for Bystander Response to Adults Who Experience Out-of-Hospital Sudden Cardiac Arrest. Circulation. 2008;117(16):2162-2167. doi:10.1161/CIRCULATIONAHA.107.189380
- Iwami Taku, Kawamura Takashi, Hiraide Atsushi, et al. Effectiveness of Bystander-Initiated Cardiac-Only Resuscitation for Patients With Out-of-Hospital Cardiac Arrest. Circulation. 2007;116(25):2900-2907. doi:10.1161/CIRCULATIONAHA.107.723411
- Katz J, Moore J. Bystander Education Training for Campus Sexual Assault Prevention: An Initial Meta-Analysis. Violence and Victims. 2013;28(6):1054-1067. doi:10.1891/0886-6708.VV-D-12-00113
- Oster-Aaland L, Lewis MA, Neighbors C, Vangsness J, Larimer ME. Alcohol Poisoning Among College Students Turning 21: Do They Recognize the Symptoms and How Do They Help? J Stud Alcohol Drugs Suppl. 2009;(s16):122-130. doi:10.15288/jsads.2009.s16.122
- Krebs, C.P., Lindquist, C.H., Warner, T.D., Fisher, B.S., & Martin, S.L. (2007). The Campus Sexual Assault (CSA) Study. Washington, DC: National Institute of Justice, U.S. Department of Justice.
- Gidycz CA, Orchowski LM, Berkowitz AD. Preventing Sexual Aggression Among College Men: An Evaluation of a Social Norms and Bystander Intervention Program. Violence Against Women. 2011;17(6):720-742. doi:10.1177/1077801211409727
- Ngo DA, Holstege C, Ding C, Miley L, Rege S. 173 Validity of Code-Based Recording of Alcohol Intoxication Among College Students Presenting to a University Hospital Emergency Department. Annals of Emergency Medicine. 2017;70(4):S69-S70. doi:10.1016/j.annemergmed.2017.07.200
- Lewis DK, Marchell TC. Safety first: A medical amnesty approach to alcohol poisoning at a U.S. university. International Journal of Drug Policy. 2006;17(4):329-338. doi:10.1016/j.drugpo.2006.02.007
- Gondi S. Tackling Barriers to Seeking Emergency Care: The Campaign for a Medical Amnesty Policy at Washington University in St. Louis. J Coll Emerg Med Serv. 2018;1(1):19-24. doi:10.30542/JCEMS.2018.01.01.04
- Megehee CM, Strick SK, Woodside AG. Overcoming Bystander Apathy and Non-Intervention in Alcohol-Poisoning Emergency Situations: Advancing Field Testing of Training-for Intervention Theory via Thought Experiments. International Journal of Business and Economics. 2012;11(2):93-103.
- Perez CE, Braslow A, Bock HC. National Standard Curriculum for Bystander Care.; 1992. Washington, DC: U.S. Dept. of Transportation, National Highway Traffic Safety Administration. //catalog.hathitrust.org/Record/005513963.
- O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. J Stud Alcohol Suppl. 2002;(s14):23-39. doi:10.15288/jsas.2002.s14.23
- Ross DW, Schullek JR, Homan MB. EMS Triage and Transport of Intoxicated Individuals to a Detoxification Facility Instead of an Emergency Department. Annals of Emergency Medicine. 2013;61(2):175-184. doi:10.1016/j.annemergmed.2012.09.004
- Pletcher MJ, Maselli J, Gonzales R. Uncomplicated alcohol intoxication in the emergency department: An analysis of the National Hospital Ambulatory Medical Care Survey. The American Journal of Medicine. 2004;117(11):863-867. doi:10.1016/j.amjmed.2004.07.042
- Leslom S, Patel S, Dezman ZDW. 64 Component Analysis of Three Screens for the Out-of-Hospital Triage of Patients With Uncomplicated Alcohol Intoxication. Annals of Emergency Medicine. 2017;70(4):S27-S28. doi:10.1016/j.annemergmed.2017.07.089
- Marco CA, Brenner JM, Kraus CK, McGrath NA, Derse AR. Refusal of Emergency Medical Treatment: Case Studies and Ethical Foundations. Annals of Emergency Medicine. 2017;70(5):696-703. doi:10.1016/j.annemergmed.2017.04.015
- New York State Bureau of Emergency Medical Services. Statewide Basic Life Support Adult and Pediatric Treatment Protocols. 2019: 1.0. https://www.health.ny.gov/professionals/ems/docs/bls_protocols.pdf. Accessed November 30, 2019.
- Prehospital Care Report (Version5). https://www.health.ny.gov/professionals/ems/pcr_5/index.htm. Accessed December 2, 2019.
- Ford C. An Introduction to Loglinear Models | University of Virginia Library Research Data Services + Sciences. University of Virginia Library. https://data.library.virginia.edu/an-introduction-to-loglinear-models/. Published July 12, 2016. Accessed December 10, 2019.
- McKillup S. Statistics Explained: An Introductory Guide for Life Scientists. 2nd ed. Cambridge: Cambridge University Press; 2011.
Author & Article Information
Bruno Di Nucci, BA, EMT-B is a recent biology graduate of Bard College and a first-year osteopathic medical student at the University of New England. He is a former member of Bard Emergency Medical Services. Adam Fallah, BA, EMT-B is a recent chemistry graduate of Bard College, currently working for the Georgia Institute of Technology’s COVID-19 research lab. He is a former member of Bard Emergency Medical Services. Anamaria Alvarez, EMT-B is a Senior psychology student at Bard College with a Concentration in Human Rights, and is a member of Bard Emergency Medical Services. Parker Smith, EMT-B is a Senior biology student at Bard College with an interest in public health and medicine, and is the Assistant Director of Bard Emergency Medical Services.
Author Affiliations: From Bard College; Bard College Emergency Medical Services – both in Annandale-on-Hudson, NY (B.D.N., A.F., A.A., P.S.).
Address for Correspondence: Bruno Di Nucci, BA, EMT-B | Email: bd1446@bard.edu / bsouzadinucci@une.edu | Phone: (347) 346-2147
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. All authors declared that they have no conflicts of interest. All authors declared that they did not receive funding to conduct the research and/or writing associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received April 16, 2019; accepted for publication July 25, 2021.
Published Online: August 10, 2021
Published in Print: August 10, 2021 (Volume 4: Issue 1)
Reviewer Information: In accordance with JCEMS editorial policy, Original Research manuscripts undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2021 Di Nucci, Fallah, Alvarez & Smith. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2021.04.01.04











