Abstract
Coronavirus Disease 2019 (COVID-19), the disease caused by the SARS-CoV-2 virus, has become a massive public health crisis causing severe acute respiratory illness in humans. Despite the rapid pace of research, much remains unknown regarding sequelae and long-term outcomes of COVID-19 due to the recency of the pandemic. We report a variant of post-COVID-19 syndrome associated with vaping an e-cigarette. A previously healthy 19-year-old university student was diagnosed with COVID-19 in July 2020. He completely recovered approximately 3 weeks later. He used an e-cigarette daily prior to infection and reported that vaping in the weeks and months post-infection caused a re-emergence of COVID-19 symptoms. He reported mild fever, pharyngitis, dyspnea, and non-productive cough persisting for an estimated two to five hours after use of an e-cigarette beginning within several hours of use. The symptoms recur consistently after use of an e-cigarette up to present day (nearly nine months post-recovery).
Introduction
A 19-year-old Asian male university student contracted COVID-19 in July of 2020 after suspected exposure at a large gathering among classmates. The patient reports e-cigarette use of approximately seven to eleven vaping sessions daily prior to his diagnosis. A nasopharyngeal swab confirmed the diagnosis that was prompted after he was informed of potential exposure to COVID-19. His COVID-19 illness was characterized by seven days of low-grade fever (101 degrees Fahrenheit), intermittent dyspnea, and temporary anosmia which all subsided within two weeks of onset. Nearly two months after recovery, the patient struggled with severe nicotine withdrawal and a reference of the array of symptoms that he experienced during his COVID-19 illness including dyspnea and fever.
In September of 2020, nearly ten weeks post COVID-19 infection, the patient presented to the emergency department (ED) for evaluation after a fall from a skateboard with right shoulder injury. He denied head trauma or loss of consciousness. The patient noted that he recovered from COVID-19 without sequelae two months prior. The patient’s physical exam was unremarkable with normal vital signs: pulse, 88/min; respiratory rate, 17 bpm; blood pressure, 124/76 mmHg; temperature, 37°C; SpO2 on room air, 99%. He was of medium build and well-appearing. Head, eyes, ears, nose, and throat (HEENT) exam was unremarkable with no apparent abrasions or lacerations. Cardiac exam was unremarkable with no cardiomegaly or thrills, regular rate and rhythm, and no apparent murmurs or gallops. There was no respiratory distress upon presentation, chest wall moved symmetrically, and clear lung sounds were appreciated on auscultation bilaterally in all lung fields. Radiologic imaging of the chest was unremarkable. Abdominal exam demonstrated normal bowel sounds, no tenderness, organomegaly, or hernia. Musculoskeletal exam demonstrated mild sternoclavicular tenderness to palpation on the right side. There was mild discomfort with passive anterior, posterior, and lateral movement of the right arm.
Just prior to discharge from the ED, he expressed concerns of “shortness of breath” that he noticed only when he vapes. His care team advised to follow-up with a pulmonologist as his reported symptomatology was not present unless an e-cigarette was used. He was provided conservative treatment for his right shoulder pain until he was able to consult his university’s team physician later in the week.
He was counseled to avoid further use of e-cigarettes and was referred to physical therapy for his acute shoulder injury. Of note, pertinent negatives from the ED and from follow-up visits thereafter include a negative rapid strep test (RST) and a high sensitivity C-reactive protein (hsCRP) within normal limits. Within one week, the patient’s fever and pulmonary complaints resolved after he tried to use an e-cigarette again after discharge and three months of unsuccessful transition back to use of the device.
In November of 2020, he was able to perform remote Pulmonary Function Testing (PFTs) utilizing a ZephyRX spirometer with a telehealth respiratory therapist post-recovery of COVID-19 to aid with data collection for this case report. Upon review, the PFTs were within normal limits. Nearly nine months after first symptom presentation, he reported that he was unable to vape and overcame nicotine dependence because of the “intolerable” side effects of vaping post-COVID-19 infection. He stated that vaping induced low-grade fever (estimated to be 101 degrees Fahrenheit), nonproductive cough, headache, and shortness of breath roughly one to two hours after any use of a vape. From what we know, this continues to be the case at present.
Complexities raised by the patient’s limited access to medical care due to his location on a college campus without transport complicated the patient’s ability to follow-up on his medical issues. Ultimately, he was seen by a pulmonologist and is yet to undergo more robust pulmonary function testing.
Discussion
We report a novel presentation of post-COVID syndrome in an otherwise healthy 19-year-old male with vaping history. The recurrent onset of fever, dyspnea, pharyngitis, and non-productive cough following the use of an e-cigarette caused significant morbidity in this patient. We explore if vaping-induced symptoms can be attributed to prior COVID-19 infection or whether the vaping-induced symptoms may just be a result of the buildup and amplified effect of this patient’s vaping history. COVID-19 might serve a role in the suspected presence of vaping associated pulmonary illness (VAPI) or, perhaps, this was facilitated simply by the patient’s continued use of vaping pre- and post-infection. Although we cannot conclude if VAPI may have occurred even without COVID-19 infection in this case, we note a possible association between vaping and COVID-19 illness.
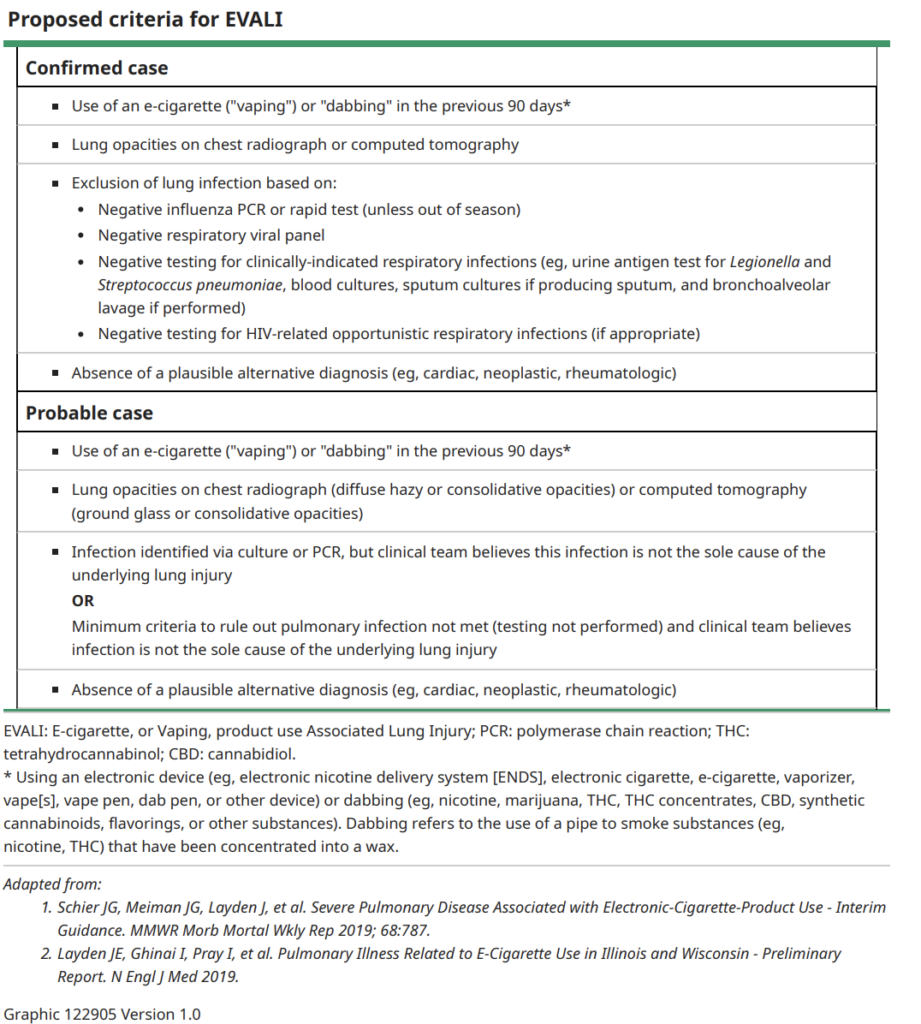
We believe this presentation represents a new variant of VAPI, sometimes referenced as an e-cigarette or vaping use-associated lung injury (EVALI) exacerbated by COVID-19 infection. Indeed, VAPI presents with a wide-ranging symptom profile, making it a challenging diagnosis.1-3 The proposed diagnostic criteria are derived from a case series of only 98 subjects as adopted from Table 1 in the VAPI summary of treatment and presentation on UpToDate. Although the literature regarding vaping and COVID-19 is still emerging, it has been reported that those using e-cigarettes are five times more likely to get COVID-19 compared to non-users.3 It is important to acknowledge that this statistic cannot imply causality due to the possibility of confounding variable; for example, the population that engages in vaping may be more inclined to engage behaviors that increase their exposure to SARS-CoV-2.4 McAlinden et al. directly suggests that vaping has not only acute cytotoxic findings but highlights the need for research on the longer-term impacts of prior COVID-19 virus exposure as a compounding risk factor for any host of pulmonary findings that are associated with respiratory diseases like VAPI or asthma.5 Our patient’s presentation offers a perspective on this condition in the new era of COVID-19. It is worth further investigating the pathological findings in those that use e-cigarettes who have contracted COVID-19 compared to those that have not contracted COVID-19. Connecting the clinical presentation in this case to a more robust understanding of possible associations with, for example, cytotoxic findings can empower the research community to explain the link between COVID-19 infection and pulmonary sequelae for patients.
Figure 1: Proposed criteria for EVALI
For EMS providers, particularly those with patient populations concentrated in a younger demographic such as on university campuses, it is critical to be aware of the possibility of atypical presentations associated with prior COVID-19 infection. Post-COVID-19 sequelae are emerging phenomena that providers have yet to fully appreciate and understand. Collegiate EMS providers should seek to incorporate a thorough history of past respiratory conditions in conjunction with COVID-19 symptoms, focusing on the presence and prevalence of vaping. The prevalence of this practice in college populations warrants further screening protocols for on-campus calls related to pulmonary distress. Trends often make it common for EMS providers to be more inclined to take history related to substance use disorder or alcohol intake, and for similar reasons due to population use, vaping use should be an added criteria for review of systems on college campuses in a post-COVID-19 world.
In synthesis, providers should consider a plethora of possible diagnoses that are beginning to present in the literature that are possibly related to COVID-19 infection. Even if patients deny typical symptomatology of fever or fatigue, the provider can sharpen their skill set with a deeper understanding of possible long-term complications that may present following recovery from COVID-19. With increasing rates of e-cigarette use on campuses, collegiate EMS organizations should also seek to keep updated on the advances in literature investigating the possible connection between e-cigarette users and COVID-19.4
References
- Richardson S, Hirsch JS, Narasimhan M, et al.: Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area (https://dx.doi.org/10.1001/jama.2020.6775). JAMA. 2020, 323:2052-2059. 10.1001/jama.2020.6775 (https://dx.doi.org/10.1001/jama.2020.6775)
- Callard F, Perego E: How and why patients made Long Covid [published online ahead of print, 2020 Oct 7] (https://dx.doi.org/10.1016/j.socscimed.2020.113426). Soc Sci Med. 2020, 113426:10.1016/j.socscimed.2020.113426 (https://dx.doi.org/10.1016/j.socscimed.2020.113426)
- The Lancet Respiratory Medicine: The EVALI outbreak and vaping in the COVID-19 era (https://dx.doi.org/10.1016/S2213-2600(20)30360-X). Lancet Respir Med. 2020, 8:831. 10.1016/S2213-2600(20)30360-X (https://dx.doi.org/10.1016/S2213-2600(20)30360-X)
- Gaiha SM, Cheng J, Halpern-Felsher B. Association Between Youth Smoking, Electronic Cigarette Use, and COVID-19. J Adolesc Health. 2020;67(4):519-523. doi:10.1016/j.jadohealth.2020.07.002
- McAlinden KD, Lu W, Ferdowsi PV, et al. Electronic Cigarette Aerosol Is Cytotoxic and Increases ACE2 Expression on Human Airway Epithelial Cells: Implications for SARS-CoV-2 (COVID-19). J Clin Med. 2021;10(5):1028. Published 2021 Mar 3. doi:10.3390/jcm10051028
- Muthumalage, T., Lamb, T., Friedman, M.R.: E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes (https://doi.org/10.1038/s41598-019-51643-6). Sci Rep. 9:19035.
- Madison MC, Landers CT, Gu BH, et al.: Electronic cigarettes disrupt lung lipid homeostasis and innate immunity independent of nicotine (https://dx.doi.org/10.1172/JCI128531). J Clin Invest. 2019, 129:4290-4304. 10.1172/JCI128531 (https://dx.doi.org/10.1172/JCI128531)
Author & Article Information
Christopher Gaeta, EMT is the Editor-in-Chief of JCEMS and a student at Swarthmore College. Joseph Zarraga, DO is currently an attending physician in the emergency department at Capitol Regional Medical Center in Tallahassee, Florida. He recently completed his residency in emergency medicine at Crozer Chester Medical Center. Joseph Cesarine, MD is a practicing emergency medicine physician at Virtua Health in Berlin, New Jersey. He is particularly interested in telehealth and digital health research.
Author Affiliations: From Children’s Hospital of Philadelphia – in Philadelphia, PA (C.G.). From Capital Regional Medical Center – in Tallahassee, FL (J.Z.). From Virtua Health – in Berlin, NJ (J.C.).
Address for Correspondence: Christopher Gaeta | Mailing Address: Swarthmore College, 500 College Ave, Swarthmore PA, 19081
Conflicts of Interest/Funding Sources: By the JCEMS Submission Declaration Form, all authors are required to disclose all potential conflicts of interest and funding sources. C.G. serves in an uncompensated editorial and managerial role for JCEMS. All authors declared that they have no conflicts of interest. All authors declared that they did not receive funding to conduct the research and/or writing associated with this work.
Authorship Criteria: By the JCEMS Submission Declaration Form, all authors are required to attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Submission History: Received November 12, 2021; accepted for publication February 7, 2022
Published Online: February 25, 2022
Published in Print: February 25, 2022 (Volume 5: Issue 1)
Reviewer Information: In accordance with JCEMS editorial policy, Case Reports undergo double-blind peer-review by at least two independent reviewers. JCEMS thanks the anonymous reviewers who contributed to the review of this work.
Copyright: © 2022 Gaeta, Zarraga & Cesarine. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0) License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The full license is available at: https://creativecommons.org/licenses/by/4.0/
Electronic Link: https://doi.org/10.30542/JCEMS.2022.05.01.02











